[ad_1]
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
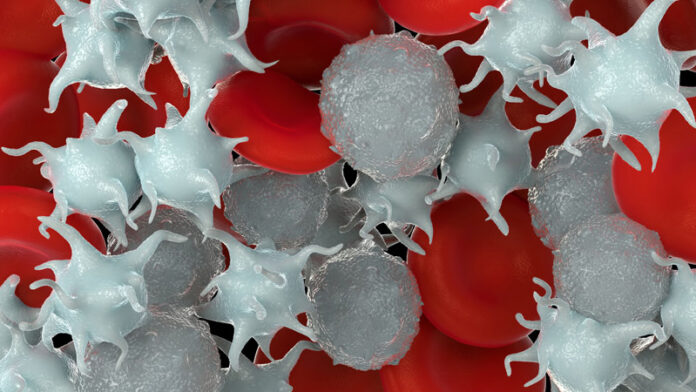
New evidence shows that COVID-19 patients with severe disease have a high level of sustained platelet activation that is likely contributing to the thrombotic issues associated with the infection.

Dr Marina Camera
“We know that COVID-19 patients have an increased thrombotic risk, despite being treated with heparin. In this study, we found evidence of a huge platelet activation in patients hospitalized with COVID-19 infection, suggesting that we should be considering antiplatelet agents as well as anticoagulants as part of their treatment,” lead author Marina Camera, PhD, told Medscape Medical News.
“Our data is important for the scientific community,” she added. “Many trials are underway investigating antiplatelet agents in COVID patients but until this study, there was no hard scientific data supporting this.”
Treating thrombotic complications in COVID-19 with anticoagulants is complicated by the high risk of bleeding if doses are increased too much, Camera noted. “These data suggest we should be trying antiplatelet agents,” she said.
Camera, who is professor of pharmacology at the University of Milan, Italy, pointed out that the findings are consistent with autopsy studies that have found platelet-rich thrombi in the microvessels of the lungs. “These thrombi get stuck in the vessels and impair oxygen exchange,” she explained.
She suggest that clinicians could consider treating patients who have a worsening COVID infection with an antiplatelet drug. “Just a low-dose aspirin — the dose used for cardiovascular prevention — could be enough. The risk would be low as it would only be taken for a few weeks,” she said, but added that more information on this would be forthcoming from the ongoing clinical trials.
But, commenting for Medscape Medical News, Prapa Kanagaratnam, PhD, professor of cardiology at Imperial College, London, UK, urged caution.
“This study is very interesting and contributes to the growing evidence to support treatment aimed at thromboprophylaxis,” Kanagaratnam said.
“It highlights the importance of supporting and completing the randomized clinical trials that are currently underway and are targeting various aspects of the thrombosis cascade. But until these trials start publishing their outcomes, we would not recommend treatment with these agents,” he added.
The study was published online in JACC: Basic to Translational Science on February 24.
The authors note that it is now well documented that severe COVID-19 infection predisposes patients to thrombotic disease, both in the venous and arterial vascular beds, which may develop despite standard pharmacologic prophylaxis with heparin.
Endothelial injury, a common feature of viral infection, can alter hemostasis directly or indirectly. Viral or bacterial infections and inflammatory stimuli can induce tissue factor expression (a key activator of the blood coagulation cascade) not only in endothelial, but also in circulating, monocytes and granulocytes; these cells upon activation also release procoagulant microvesicles into the bloodstream, the authors explain.
Platelets participate in inflammation and thrombotic responses in many viral
infections, the researchers report. “The low platelet count often described
in COVID-19 patients suggests increased consumption due to a massive platelet activation and thrombus formation. Activated platelets also express a functionally active tissue factor so they are able themselves to trigger the coagulation cascade,” they write.
Severe COVID-19 is also associated with a cytokine storm, but how this affects platelet and endothelial activation in this clinical setting is almost completely unknown, they note. “Whereas data are rapidly emerging about COVID-19–associated coagulopathy and thrombosis risk, there is little high-quality evidence to guide antithrombotic management,” they add.
The current study involved analysis of blood from 46 consecutive COVID-19 patients admitted to San Luca Hospital, Milan, in April 2020. The researchers assessed the level of tissue factor expression among the circulating cells and microvesicles; the residual plasma thrombin generation capacity despite heparin treatment; and the extent of platelet and endothelial activation.
They report “a massive cell activation with production of tissue factor, mainly by platelets, granulocytes, and microvesicles.”
The median level of TF+ platelets in COVID-19 patients was significantly higher than that found in healthy participants, with a trend toward greater values in COVID patients needing ventilation compared with those not needing ventilation.
Results also showed a sustained platelet activation in terms of P-selectin expression and platelet–leukocyte aggregate (PLA) formation, and altered nitric oxide/prostacyclin synthesis.
When plasma from the COVID-19 patients was added to the blood of healthy subjects, platelet activation similar to that observed in vivo was seen. This effect was blunted by pre-incubation with aspirin, a P2Y12 inhibitor or the interleukin-6 (IL-6) antibody tocilizumab (Actemra).
“These observations give insights into the IL-6–mediated platelet activation that triggers the hypercoagulable state in COVID-19, suggesting the potential effectiveness of anti–IL-6 antibodies and antiplatelet drugs,” the authors write.
“The present study provides, for the first time to our knowledge, evidence that the coagulopathy reported in COVID-19 patients is supported by: 1) a sustained tissue factor expression by virtually all the cells in contact with blood and by the derived microvesicles; and 2) a massive platelet activation characterized by the formation of PLA that may be involved in the pulmonary microthrombi found in autoptic specimens,” the researchers state.
“Our data provide the bench-to-clinic rationale behind the ongoing clinical trials assessing the potential effectiveness of antiplatelet drugs and IL-6 receptor antagonists in the treatment of COVID-19 patients,” they add.
This work was supported by a grant from Italian Ministry of Health. The authors have disclosed no relevant financial relationships.
JACC: Basic to Translational Science. Published online February 24, 2021. Full text
For more Medscape Neurology news, join us on Facebook and Twitter
[ad_2]
Source link