[ad_1]
Among patients who have recently experienced an ischemic stroke thought to be caused by small-vessel occlusion or large-vessel atherosclerosis, atrial fibrillation (AF) is detected more often with an insertable cardiac monitor (ICM) than with standard of care, a new study shows.
ICMs may detect AF in as many as 1 in 8 patients with stroke of this etiology, the researchers report. The findings, from the STROKE-AF trial, were presented at the International Stroke Conference (ISC) 2021.
The data show that AF is more common with these stroke subtypes than previously suspected, said Lee H. Schwamm, MD, executive vice chairman of the Department of Neurology at Massachusetts General Hospital, Boston, Massachusetts, during his presentation.
“We’re really trying with this study to move away from the reliance on our initial probabilistic estimate of the cause of the stroke but rather to envision a world where we identify patients who may be at risk of ischemic stroke and in whom the presence of AF would dramatically change our decision about future treatment,” Schwamm said.
Since publication of the CRYSTAL-AF study, the use of an ICM to detect AF in patients with stroke of unknown cause (cryptogenic stroke) has become common. In that study, ICM detected AF in 12.4% of patients during a 12-month period. Approximately 23% of patients who have had a first stroke have recurrent stroke, for which AF is a risk factor.
Guidelines for the prevention of secondary stroke do not recommend long-term monitoring for AF for patients with ischemic stroke attributed to large-artery atherosclerosis or small-vessel occlusion. The researchers conducted their investigation to determine the rate of AF in this population, as well as to analyze whether ICMs detect AF more so than the standard of care does.
Table of Contents
Long Episodes
The STROKE-AF trial was a prospective, randomized, controlled study in which 33 US centers collaborated. Eligible participants had no history of AF diagnosis, were 60 years of age or older, had had an index stroke 10 or fewer days before ICM insertion, and had no contraindication to long-term oral anticoagulation. Patients aged 50 to 59 years also were eligible if they had an additional stroke risk factor, such as hypertension or congestive heart failure.
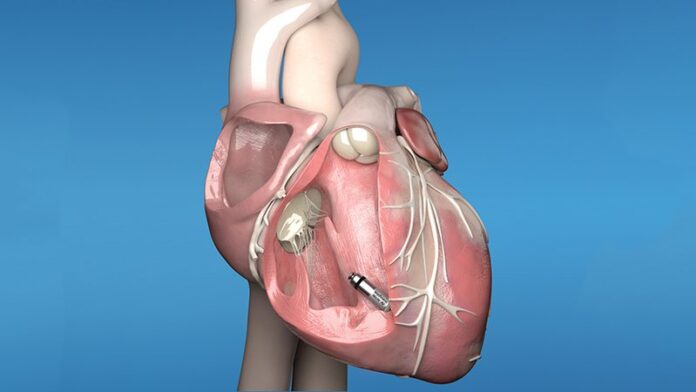
Participants were randomly assigned to receive an ICM or site-specific standard of care for the detection of AF. The ICM device detects episodes of AF lasting at least 2 minutes. Episodes of AF were adjudicated by a clinical events committee.
The researchers’ primary goal was to compare the AF incidence rate at 12 months among the patients who received ICMs with the rate among those who received standard of care. A subgroup analysis compared the incidence rates of AF in the two study arms with respect to stroke subtypes. The researchers plan to conduct secondary analyses at 3 years.
They enrolled 496 participants, of whom 242 were randomly assigned to receive an ICM and 250 to standard of care. There were no significant differences in baseline characteristics between the study arms. The mean age was 67 years, and 62% of the population was male. The median CHA2DS2-VASc score was 5, indicating significant stroke risk among patients for whom AF was detected.
At 12 months, AF was detected in 12.1% of patients in the ICM arm and in 1.8% of patients who received standard of care (hazard ratio [HR], 7.41; P < .001).
The median time to first detection of AF in the ICM arm was 99 days. The rate of detected AF within the first 30 days was 2.6% in the ICM arm and 0.4% in the standard-of-care arm.
Among patients with ICMs, the rate of AF detection was similar regardless of whether stroke resulted from large-artery atherosclerosis (11.7%) or small-vessel occlusion (12.6%). In the ICM arm, 55.5% of patients in whom AF was detected experienced an episode that lasted more than 1 hour. About 44% of patients experienced an episode that lasted more than 4 hours. About 96% of first AF episodes were asymptomatic.
Oral anticoagulation was prescribed to prevent recurrent stroke in a greater proportion of those with AF in the ICM arm (7.4%) than in the standard-of-care arm (1.2%).
In addition, there were fewer recurrent strokes in the ICM arm (15 vs 23; HR, 0.67; P = .23).
“Thirty days of ambulatory cardiac monitoring, which is a common practice in the United States, even among patients with cryptogenic stroke, would have been insufficient to capture the vast majority of AF episodes that occurred in this trial,” said Schwamm. “Clearly, use of ICM in this population may be beneficial to detect poststroke AF and to inform optimal stroke prevention strategies.”
No Control Group
“This is an interesting study that shows that when we look more systematically with ICMs, the occurrence of undiagnosed AF is more frequent than we originally thought among stroke patients with large-artery atherosclerosis and small-vessel disease,” Ralph L. Sacco, MD, professor and Olemberg Chair of Neurology at the University of Miami, Coral Gables, Florida, told Medscape Medical News.

Dr Ralph Sacco
Previous research has indicated that AF occurs more frequently among patients with cryptogenic stroke, especially when a possible embolic mechanism is suspected, he said.
ICMs are reasonably accurate but can miss AF episodes that last less than 2 minutes, said Sacco. Stroke patients with AF of very short duration therefore could have been undercounted in this study.
The study’s biggest limitation is its lack of a control group, said Sacco.
“We know that the risk of AF goes up markedly with age and is associated with other vascular risk factors and cardiac comorbidities that could coexist in patients with large-vessel disease, as well as small-vessel disease,” he said. “If we monitor many nonstroke patients with ICMs who are older and have other vascular risk factors, we may also detect more underrecognized AF.”
In addition, further critical review of the study is needed before its findings will influence clinical practice, said Sacco. “While I agree that finding AF would likely change management even if the AF was not related to the initial stroke, we will need to evaluate the cost efficiency of more widespread ICM use.”
The study was funded by Medtronic. Schwamm has received compensation from Medtronic, Penumbra, LifeImage, and Genentech. Sacco receives support from the AHA as editor in chief of Stroke.
International Stroke Conference (ISC) 2021: Late-breaking abstract 6. Presented March 18, 2021.
For more Medscape Neurology news, join us on Facebook and Twitter.
[ad_2]
Source link