[ad_1]
The presence of ischemia on stress testing should not be used to refer patients with ischemic cardiomyopathy for coronary artery bypass graft (CABG) surgery, a new STICH analysis concludes.
Previously, the Surgical Treatment for Ischemic Heart Failure (STICH) trial showed that CABG plus medical therapy provided no mortality benefit over medical therapy at 5 years, but significantly reduced mortality out to 10 years in patients with multivessel coronary artery disease (CAD) and a left ventricular ejection fraction less than 35%.
Inducible ischemia at baseline was not associated with greater mortality or a mortality reduction from CABG at 5 years and, now with longer follow-up, even at 10 years.
“These findings run counter to decades of accumulating dogma suggesting a causal relationship between ischemia and adverse outcomes, including mortality, and to the belief that ischemia identifies patients in whom revascularization improves outcomes,” Kevin O’Fee, MD, Washington University School of Medicine, St. Louis, and colleagues write in the research letter published in the January 12 issue of Circulation.
The analysis also extends the findings of the ISCHEMIA trial to patients with severe left ventricular dysfunction, the authors note. That trial shook the cardiology world last year with the finding that outcomes were not significantly better with an initial invasive approach than with medical therapy in stable patients with CAD and moderate or severe ischemia.
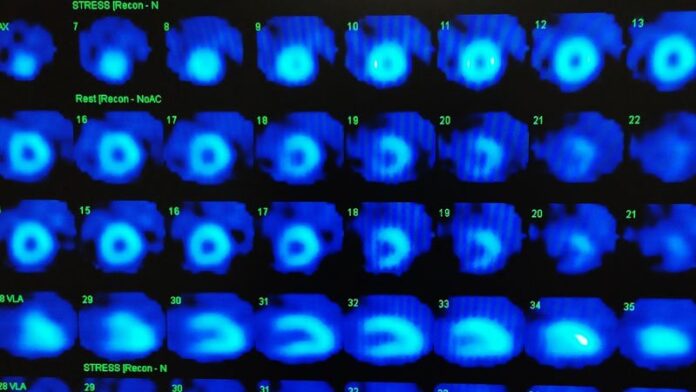
Although ischemia testing was not required in STICH, 402 of the 1212 randomized patients underwent baseline radionuclide or echocardiographic stress tests. They were slightly older (mean, 61 years) and had a lower ejection fraction (mean, 26%) but less likely to have advanced angina or heart failure.
All-cause mortality at 10 years was similar between those who did and did not undergo stress testing (66% vs 61%; adjusted hazard ratio [aHR], 0.95; 95% CI, 0.81 – 1.11).
Among the 402 patients with stress testing, 63% had inducible ischemia (mean, 18% ischemic myocardium) and 37% did not.
Neither the presence nor the extent of ischemia was associated with higher all-cause mortality at 10 years when analyzed as a dichotomous (69% with ischemia died vs 61% without ischemia; aHR, 1.21; 95% CI, 0.93 – 1.58) or continuous (aHR, 1.89; 95% CI, 0.66 – 5.40) variable.
There was a trend toward lower mortality with CABG that did not achieve statistical significance with ischemia as a dichotomous (55% vs 67%; aHR, 0.79; 95% CI, 0.62 – 1.01) or continuous (aHR, 0.80; 95% CI; 0.63 – 1.03) variable.
There was no significant interaction between randomization to CABG and the presence or extent of ischemia, either as a dichotomous (P = .62) or continuous (P = .52) variable.
“When you take it all together, what it suggests to me is that the benefit of CABG is kind of like the benefit of an ICD. It’s an insurance policy that protects you should you have a heart attack in one of your native vessels by providing an alternative conduit blood flow,” coauthor David L. Brown, MD, also from Washington University School of Medicine, said in an interview. “These people are living with such a low ejection fraction that if they have a heart attack of any significant size, they aren’t going to survive.”
He noted that there are few data on the merits of percutaneous coronary intervention (PCI) for ischemic cardiomyopathy but that the ongoing REVIVED-BCIS2 trial should provide insights.
Brown and colleagues published a new meta-analysis last week of seven randomized trials — including STICH, ISCHEMIA, and ISCHEMIA-CKD, with more than 10,000 patients with chronic coronary syndromes and myocardial ischemia — in which initial revascularization with CABG or PCI provided no mortality benefit over medical therapy at a median of 5 years. In subgroup analysis, however, nonfatal MI was significantly lower with CABG but not with PCI.
Although the ISCHEMIA trial challenged existing dogma, there is still a strong belief in cardiology, on the basis of early trials like the CAST study, that revascularization in patients with coronary disease and low ejection fraction is mandatory, James Januzzi, MD, Massachusetts General Hospital and Harvard Medical School, Boston, told theheart.org | Medscape Cardiology. “This analysis, which is by no means definitive but nonetheless provocative, calls that somewhat into question.”
“What this says is that the mere presence of ischemia alone should not be utilized as the only decision point for whether or not a patient with a low ejection fraction should be revascularized,” he said. “It should be based on the global picture, including the risks of surgical revascularization, the presence or absence of symptoms of coronary ischemia, and, of course, the stability or instability of heart failure that may be present.”
Although this is a post hoc, retrospective analysis of a very small number of patients, “its consistency with the results from ISCHEMIA study really merits consideration for a follow-up randomized trial to better understand how to manage these very complicated patients,” Januzzi said.
The STICH trial was supported by the National Heart, Lung, and Blood Institute. The authors and Januzzi reported no relevant disclosures.
Circulation. 2021;143:205-207. Full text
Follow Patrice Wendling on Twitter: @pwendl. For more from theheart.org | Medscape Cardiology, join us on Twitter and Facebook.
[ad_2]
Source link